Drop Date: October 2023
Salivary Cortisol: Could it be our collective research focus has been too narrow?
In This Drop: Salivary Cortisol: Could it be our collective research focus has been too narrow?
By: Kristina Feghali and Douglas A. Granger
If you are interested in the relationship between stress, biology, and behavior, you are probably aware of how salivary cortisol has been integrated into applied research to represent the activity of the hypothalamic-pituitary-adrenal axis (HPA) component of the psychobiology of the stress response. Generally summarizing, cortisol levels increase in response to novelty when situations are unfamiliar, and the individual has minimal prior experience to respond and adapt. Higher cortisol levels are also associated with social withdrawal, negative affect, and psychological distress. The literature documenting these associations is extensive.
So much research effort has been focused on cortisol as a measure of stress that the key role cortisol plays in metabolism has been overlooked in many of these publications. Cortisol’s role in metabolism provides important mechanistic connectivity to health and disease. Incorporating these relationships into studies of salivary cortisol, stress, and behavior translates basic descriptive work into high-impact, meaningful outcomes.
Expanding the Scope: Cortisol, Glucose, and Insulin
Any search engine will summarize these relationships, so only a short teaser is provided here. Cortisol’s primary role in physiology is to mobilize glucose into the circulation from energy stores. Cortisol provides the body with glucose through the process of gluconeogenesis in the liver. Indeed, when cortisol rises in response to stress, the primary reason is to raise glucose levels that enable the individual to have the energy to respond to the immediate challenge. Having chronically high cortisol levels can reduce the effectiveness of insulin in lowering blood sugar and lead to insulin resistance, hyperglycemia, and risk for type 2 diabetes. Including measures of glucose and insulin in studies of salivary cortisol reactivity and recovery from stress seems well justified.
The main function of insulin is to enable cells to absorb glucose from the blood. The development of insulin resistance necessitates an increase in insulin production to sustain healthy blood sugar levels.
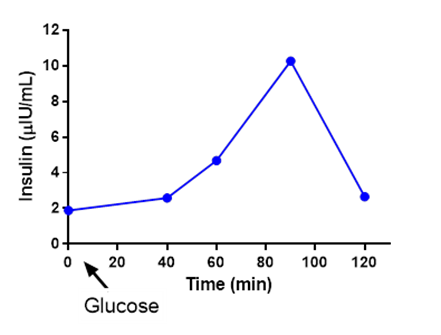
| Figure 1: Healthy salivary insulin reactivity and recovery to ingestion of 35g sugar. Timing started immediately after glucose was ingested. |
Insulin functions to store and use energy, while cortisol functions to rapidly gain access to energy. Cortisol can reduce the effectiveness of insulin, which makes sense because the body is working to create energy, and the last thing it needs is insulin to reduce it. Lowering cortisol through stress management and other methods may help regulate insulin secretion and blood glucose levels.
New Considerations and Perspective
Does anybody suspect that the cognitive and behavioral correlates of cortisol responses to stress might be mediated by cortisol-induced changes in glucose? Has anyone considered that the magnitude of the cortisol response to a stressor might be moderated by glucose levels or insulin levels pre-challenge? Has anybody included hyper or hypo-glycemia or -insulinemia as blocking or exclusionary variables in their studies of salivary cortisol reactivity and recovery to stress?
For the past five years, Salimetrics has been working on methods to enable the measurement of glucose and insulin in saliva. Our goal is to enable the integration of these measures in future studies in an effort to advance our understanding of the literature linking stress, salivary cortisol, and behavior in important ways. For instance, this literature consistently reveals that individual differences are the norm rather than the exception. We hypothesize this is partially due to incomplete operationalization of cortisol biology. Incorporating insulin and glucose in the next generation of our measurement models should enable us to test links between salivary cortisol and specific and important issues (i.e., diabetes) affecting human health and development.
Is it possible that the salivary cortisol literature has focused too narrowly on cortisol as an index of stress? We encourage research teams to think so, and we encourage integrating a more comprehensive understanding of cortisol biology into the next generation of studies.
Empowering You
Let us share our expertise with you. Let us connect you to others who are already engaged in this effort. Let us provide the tools and support you need to develop and test research questions related to this important issue. Take a minute and explore the wide range of funding opportunities, public and private, afforded to you by expanding your research focus in this direction.
So you know, salivary insulin, glucose, and cortisol can be analyzed from the same saliva sample collection, and the added test volume requirements are minimal. To get started, connect with us, and we will be happy to help.
REFERENCES & RELATED RESEARCH
*Note: Salimetrics provides this information for research use only (RUO). Information is not provided to promote off-label use of medical devices. Please consult the full-text article.
 Contact: Salimetrics (USA)
Contact: Salimetrics (USA)