Drop Date: February 2011
SBB – Stress, the HPA Axis and Aging
In This Drop: Stress, the HPA Axis and Aging
 As populations around the world grow increasingly older, the study of factors that can lead to unhealthy aging has become an important focus in bio-behavioral research. In particular, the ever-present psychological and physical stress found in modern societies is thought to be a major environmental factor that can accelerate the aging process, as well as being involved in increases in related diseases such as hypertension, type II diabetes, osteoporosis, cardio-vascular disease, and stroke. Acting largely through two well-known systems, the hypothalamic-pituitary-adrenal (HPA) axis, and the sympathetic-adrenal-medullary (SAM) axis, stress can have an effect on numerous other interlinked systems throughout the body, with important consequences for aging and diseases related to aging.
As populations around the world grow increasingly older, the study of factors that can lead to unhealthy aging has become an important focus in bio-behavioral research. In particular, the ever-present psychological and physical stress found in modern societies is thought to be a major environmental factor that can accelerate the aging process, as well as being involved in increases in related diseases such as hypertension, type II diabetes, osteoporosis, cardio-vascular disease, and stroke. Acting largely through two well-known systems, the hypothalamic-pituitary-adrenal (HPA) axis, and the sympathetic-adrenal-medullary (SAM) axis, stress can have an effect on numerous other interlinked systems throughout the body, with important consequences for aging and diseases related to aging.
In this edition of The Salivary Bioscience Bulletin, we begin an examination of this topic by first looking at the HPA axis and related systems. The research presented here includes prominent discussions of three of the major hormone end-products of the HPA axis – cortisol, dehydroepiandrosterone (DHEA), and dehydroepiandrosterone sulfate (DHEA-S) – which are thought to be key players in the process of aging.
Featured Article
Depression Gets Old Fast: Do Stress and Depression Accelerate Cell Aging?
Wolkowitz, O.M., Epel, E.S., Reus, V.I., & Mellon, S.H. (2010). Depress Anxiety, 27(4), 327-38.
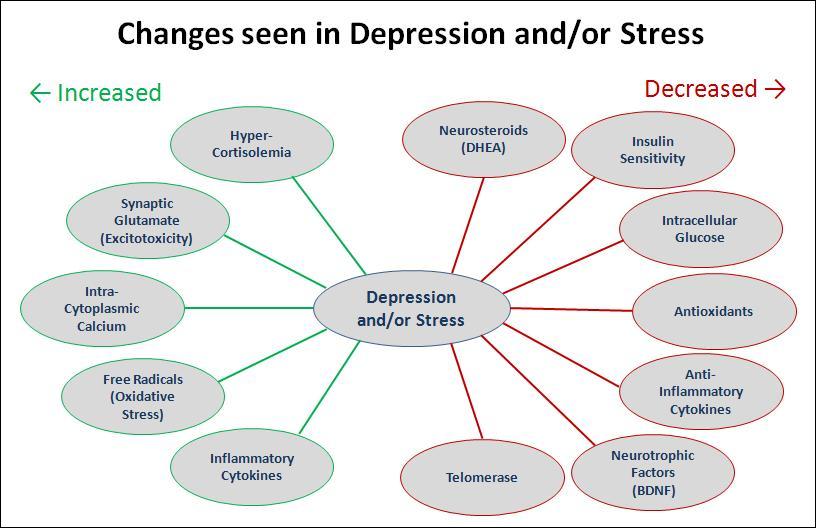
It has been generally recognized that major depression can have a serious impact on the health of the brain and other systems throughout the body. Depressed individuals are known to have higher rates of diseases associated with aging, such as diabetes, osteoporosis, heart disease, stroke, and cognitive problems, as well as elevated risk for early mortality. In this review, the authors present an updated theoretical model of depression that links together details of HPA axis regulation and its effects on other systems in the body, including immune function, protection against oxidative stress, neuroprotective factors, and preservation of DNA integrity. Although the focus of this review is the relationship between major depression and aging, significant portions of it are relevant to the general discussion of stress-related changes that occur with aging, as well as to psychological conditions other than depression.
Since major depression is often accompanied by elevated levels of glucocorticoids (GC), principally cortisol, the review begins by considering the physiological implications of altered GC levels. It is pointed out that, even when circulating cortisol levels are elevated, the net level of cortisol signaling within cells may be either low or high. The hypo-cortisolism hypothesis predicts that individuals who have lowered glucocorticoid receptor (GR) activity will have GC resistance – a net reduction in cortisol signaling within the cell. The GC resistance can be caused by GR polymorphisms or by down-regulation of GR activity due to excessively high cortisol levels that accompanied adverse early-life events. High circulating cortisol levels in these individuals may therefore be an attempt by the body to counteract the GC resistance. In contrast, the hyper-cortisolism hypothesis predicts that individuals who have both elevated levels of circulating cortisol and higher levels of GR activity will show signs of over-active intra-cellular cortisol signaling. Operating through various genomic and non-genomic mechanisms, both elevated and depressed levels of GC activity can lead to behavioral changes and cellular damage. In particular, individuals in the hyper-cortisolism group are thought to be vulnerable to diseases such as osteoporosis, insulin resistance, type II diabetes, and metabolic syndrome, which are a major concern in aged populations. The authors also note that these hormone-cell relationships are complex, and that the effects of hypo- or hyper-cortisolism at the cellular level may even be present at the same time in an individual, depending on the expression of specific receptors or metabolic enzymes in the various tissues that are involved. It is possible, but not yet proven, that hypo- and hyper-cortisolism may identify different subtypes of depression, or be related to different symptom clusters.
Because the immune system is heavily influenced by HPA axis activity, it is thought that immune dysregulation may be a major pathway through which depression and stress heighten the risk of serious medical conditions. Depressed individuals often have elevated levels of pro-inflammatory cytokines accompanied by reduced levels of anti-inflammatory cytokines. This shift in the ratio of pro- to anti-inflammatory mediators may result in a state of elevated inflammation that is accompanied by increased free-radical damage to proteins, lipids, and DNA in many tissues. The brain is especially sensitive to such oxidative damage. Elevated levels of pro-inflammatory cytokines also reciprocally lead to further alterations in HPA axis activity, heightening the effects of the stress response.
At the same time that inflammatory levels are increased in depression and aging, levels of the protective neurosteroids dehydroepiandrosterone (DHEA) and allopregnenolone are decreased. DHEA has been investigated in particular for its ability to counteract the effects of hyper-cortisolism, and it has been shown to have significant antidepressant effects. Prolonged stress and high levels of cortisol can also down-regulate levels of brain-derived neurotropic factor (BDNF), which serves an important neuroprotective and anti-inflammatory role in nervous tissues.
A final cause of accelerated cellular aging discussed in the review involves telomeres, which are DNA-protein complexes that protect the ends of linear DNA strands during cell division. Telomeres can be damaged by repeated divisions without adequate presence of telomerase, the enzyme that rebuilds telomere length, or by oxidative damage from elevated levels of free radicals. Reduced telomerase activity and shortening of telomeres can be related to changes in levels of cortisol, oxidative stress, and inflammatory cytokines, along with environmental factors such as childhood maltreatment, socioeconomic status, and physical exercise.
The authors clearly state that the hypothetical model in this presentation is not meant to be complete or all-encompassing, and that it will not apply to all individuals with major depression. Rather, the intent was to highlight some interesting recent findings and to incorporate them into a broadly-painted overview of stress and depression, which will hopefully stimulate and guide future research.
REFERENCES & RELATED RESEARCH
Socio-Economic Differentials in Peripheral Biology: Cumulative Allostatic Load
Martin, S.A., Grandt, D.P., Woods, J.A. Exerc Sport Sci Rev 37(4) (2009): 157-64.
In a series of earlier papers by the authors, the concept of allostatic load – a measure of the cumulative physiological burden exacted on the body through attempts to adapt to life’s demands – has been introduced and developed. In this discussion they consider the negative effects on health and aging that can result from dysregulation of physiological systems in response to adverse social conditions. Assessment of allostatic load involves measurement of multiple biomarkers, which represent the cardiovascular, metabolic, HPA axis, autonomic nervous, and inflammatory systems. The steroid hormones cortisol and DHEA-S are included as measures of activity in the HPA axis.
Identifying Patterns in Cortisol Secretion in an Older Population: Findings from the Whitehall II Study
Kumari, M., Badrick, E., Sacker, A., Kirschbaum, C., Marmot, M., & Chandola, T. (2010). Psychoneuroendocrinology, 35(7), 1091-9.
In contrast to the normal diurnal variation for cortisol in healthy individuals, which features high levels in the morning, a peak in production shortly after awakening, and then a steady decline to lowest levels in the late evening, a number of altered patterns have been observed in connection with various psychiatric conditions. These include long-lasting depression, where evening levels do not decline as usual, and chronic fatigue, which is associated with low, flat curves with relatively little variation over the day. In this large study (n=2802), saliva samples were collected at six time points over the course of a day and analyzed for cortisol. Participants (mean age 60.9 year) also provided a self assessment of their stress level on that day, and their walking/gait speed was measured. Using a latent class analysis approach, the study found two basic patterns: a normative curve and a raised curve. The raised curve, which exhibited a higher diurnal level with slower decline over the day, was associated with older age, being male or a smoker, stress on the day of sampling, slower walking speed, and shorter sleep duration.
Cardiovascular Disease is Associated with Greater Incident Dehydroepiandrosterone Sulfate Decline in the Oldest Old: The Cardiovascular Health Study All Stars Study
Sanders, J.L., Boudreau, R.M., Cappola, A.R., Arnold, A.M., Robbins, J., Cushman, M., & Newman, A.B. (2010). J Am Geriatr Soc, 58(3), 421-26.
The CHS-All Stars study is a four-center, longitudinal, observational, community-based study of the onset, progression, and course of cardiovascular disease in 5,888 men and women (65 or older), which began in 1989/90. Information collected at clinical visits included demographics, vital signs, anthropometric factors, medical history and behaviors, physical function, and psychosocial interviews. Using blood samples collected from 989 of these participants in 1996/97 (mean age 76.3) and again in 2005/06 (mean age 85.2), this paper examines changes in plasma DHEA-S levels in relation to health status. This study with a very old population confirms previous reports that DHEA-S levels are generally lower in women and that they continue to decrease with age. However, the effect of sex was largely attenuated by the age of 79. Additionally, cardiovascular disease was found to be associated with greater change in DHEA-S levels. The authors discuss the differences based on sex, possible interpretations of the association with CVD, and the general value of DHEA-S as a marker of aging.
*Note: Salimetrics provides this information for research use only (RUO). Information is not provided to promote off-label use of medical devices. Please consult the full-text article.
 Contact: Salimetrics (USA)
Contact: Salimetrics (USA)