Salimetrics Assay #1-1252
The Salimetrics Salivary DHEA-S (DHEA-Sulfate) Enzyme Immunoassay Kit was specifically designed to standardize the detection of DHEA-S in saliva samples for research and biomedical laboratories. Using a small sample volume, this assay kit has an extended range which spans the expected DHEA-S levels found in human saliva. The average inter- and intra-assay precision coefficients of variation are low with no deleterious matrix effects often found in saliva which are characterized through dilution- and spike-recovery validation procedures. This DHEA-S assay kit has also been formatted to minimize cross reactivity for related steroids. Read More...DHEA-S is the most abundant steroid hormone in humans, with circulating concentrations approximately 250 and 500 times higher than those of its unsulfated analog, DHEA, in women and men, respectively. DHEA-S is not bound by sex hormone binding globulin (SHBG) in the blood stream and is readily available for conversion to other compounds. Unlike DHEA, DHEA-S does not normally exhibit any diurnal pattern of secretion and DHEA-S concentrations in saliva decrease markedly as flow rates increase. Levels of DHEA-S peak around the age of 20 to 30, and then decline to only 20-30% of peak levels by the age of 70 to 80. Critical illness and emotional or physical stress can also cause DHEA-S levels to decline. DHEA-S and DHEA are also synthesized directly by the central nervous system, where they appear to help protect nervous tissue against harmful agents. DHEA-S is not lipid soluble, and it cannot enter saliva by passive diffusion through cell membranes like most of the other steroid hormones. Instead, it enters saliva only by squeezing through the tight junctions between cells in the saliva glands, and it is too large to do this readily. It is therefore present in relatively small amounts. Binding proteins or enzymes in saliva that would affect the measurement of free DHEA-S appear largely to be absent.
Technical Summary
| Assay Protocol |
|---|
| Rev. 09.09.22
|
| Specifications | |
|---|---|
| Catalog#: | 1-1252 |
| Regulatory Status: | RUO |
| Format: | 96-well plate |
| Assay Time: | ~ 2 hrs |
| Sample Volume/Test: | 100 µL |
| Sensitivity: | 95.14 pg/mL |
| Assay Range: | 188.9 pg/mL- 15,300 pg/mL |
| Storage Requirements: | 2-8°C |
| Tests Per Kit | |
|---|---|
| Singlet: | 76 |
| Duplicate: | 38 |
| Target Analyte |
|---|
| Technical Documentation |
|---|
Salivary DHEA-S Assay Kit Overview
Intended Use
The Salimetrics DHEA-S Enzyme Immunoassay Kit is a competitive immunoassay specifically designed and validated for the quantitative measurement of salivary DHEA-S. It is not intended for diagnostic use. It is intended only for research use in humans and some animals. Salimetrics has not validated this kit for serum or plasma samples.
Introduction
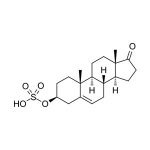
Dehydroepiandrosterone-sulfate (DHEA-S) is a steroid hormone produced primarily in the adrenal cortex. DHEA-S is the most abundant steroid hormone in humans, with circulating concentrations approximately 250 and 500 times higher than those of its unsulfated analog, DHEA, in women and men, respectively. DHEA-S serves as a precursor molecule that is circulated to various target tissues in the body. In those locations the sulfate is removed to yield DHEA, and the DHEA is then further metabolized into various estrogenic and androgenic compounds. DHEA-S is not bound by sex hormone binding globulin (SHBG) in the blood stream and is readily available for conversion to other compounds. Unlike DHEA, DHEA-S does not normally exhibit any diurnal pattern of secretion. Levels of DHEA-S peak around the age of 20 to 30, and then decline to only 20-30% of peak levels by the age of 70 to 80. Critical illness and emotional or physical stress can also cause DHEA-S levels to decline. Lowered DHEA-S levels have been linked with a variety of medical conditions. DHEA-S and DHEA are also synthesized directly in the central nervous system, where they appear to help protect nervous tissue against harmful agents. Studies have begun to explore possible relationships between DHEA-S levels and changes in neurological function, including sense of well-being, cognition, depression, and various other psychiatric disorders. DHEA-S is not lipid soluble, and it cannot enter saliva by passive diffusion through cell membranes like most of the other steroid hormones. Instead, it enters saliva only by squeezing through the tight junctions between cells in the saliva glands, and it is too large to do this readily. It is therefore present in relatively small amounts. Binding proteins or enzymes in saliva that would affect the measurement of free DHEA-S appear largely to be absent. DHEA-S levels measured in whole saliva may be inaccurate if contamination by plasma exudates from the gums or from small injuries in the mouth is present. Subjects should be carefully screened for periodontal disease and advised about proper collection procedures. Saliva may also be screened for blood contamination using the Salimetrics Blood Contamination EIA Kit (Item. No. 1-1302). DHEA-S concentrations in saliva decrease markedly as flow rates increase.
Salivary DHEA-S Assay Principle
This is a competitive immunoassay kit. DHEA-S in standards and samples compete with DHEA-S conjugated to horseradish peroxidase for the antibody binding sites on a microtitre plate. After incubation, unbound components are washed away. Bound DHEA-S Enzyme Conjugate is measured by the reaction of the horseradish peroxidase enzyme to the substrate tetramethylbenzidine (TMB). This reaction produces a blue color. A yellow color is formed after stopping the reaction with an acidic solution. The optical density is read on a standard plate reader at 450 nm. The amount of DHEA-S Enzyme Conjugate detected is inversely proportional to the amount of DHEA-S present in the sample.
References & Salivary DHEA-S Rsearch
-
- Summarized in Whetzel, C.A., Klein, L.C. Measuring DHEA-S in saliva: Time of day differences and positive correlations between two different types of collection methods. BMC Res Notes, 3:204.
- Krobath, P.D., Salek, F.S., Pittenger, A.L. et al. (1999). DHEA and DHEA-S: A review. J Clin Pharmacol 39(4), 327-48.
- Rosenfeld, R.S., Rosenberg, B.J., Fukushima, D.K., Hellman, L. (1975). 24-Hour secretory pattern of dehydroisoandrosterone and dehydroisoandrosterone sulfate. J Clin Endocrinol Metab, 40(5), 850-55.
- Carlström, K., Karlsson, R., Von Schoultz, B. (2002). Diurnal rhythm and effects of oral contraceptives on serum dehydroepiandrosterone sulfate (DHEAS) are related to alterations in serum albumin rather than to changes in adrenocortical steroid secretion. Scan J Clin Lab Invest, 62(5), 361-68.
- Labrie, F., Bélanger, A., Cusan, L., Candas, B. (1997). Physiological changes in dehydroepiandrosterone are not reflected by serum levels of active androgens and estrogens but of their metabolites: Intracrinology. J Clin Endocrinol Metab, 82(8), 2403-9.
- Labrie, F., Luu-The, V. Bélanger, A., et al. (2005). Is dehydroepiandrosterone a hormone? J Endocrinol, 187, 169-96.
- Charalampopoulos, I., Alexaki, V.-I., Tsatsanis, C., et al. (2006). Neurosteroids as endogenous inhibitors of neuronal cell apoptosis in aging. Ann N Y Acad Science, 1088, 138-52.
- Baulieu, E.-E., Robel, P. (1998). Dehydroepiandrosterone (DHEA) and dehydroepiandrosterone sulfate (DHEAS) as neuroactive neurosteroids. Proc Natl Acad Sci U S A, 95(8), 4089-91.)
- Kellner, M., Muhtz, C., Peter, F., et al. (2010). Increased DHEA and DHEA-S plasma levels in patients with post-traumatic stress disorder and a history of childhood abuse. J Psychiatr Res, 44(4), 215-9.
- Golubchik, P., Mozes, T., Maayan, R., Weizman, A. (2009). Neurosteroid blood levels in delinquent adolescent boys with conduct disorder. Eur Neuropsychopharmacol, 19(1), 49-52.
-
- Azurmendi, A., Braza, F., Garcia, F. et al. (2006). Aggression, dominance and affiliation: Their relationships with androgen levels and intelligence in 5-year-old children. Horm Behav, 50(1), 132-40.
- MacLaughlin, B.W., Wang, D., Noone, A.-M., et al. (2010). Stress biomarkers in medical students participating in a mind body medicine skills program. eCAM, doi:10.1093/ecam/neq039.
- Wang, J.-S., Chen, S.-M., Lee, S.-P., et al. 2009). Dehydroepiandrosterone sulfate linked to physiologic response against hot spring immersion. Steroids, 74(12), 945-49.
- Vining, R.F., McGinley, R.A., Symons, R.G. (1983). Hormones in saliva: Mode of entry and consequent implications for clinical interpretation. Clin Chem, 29(10), 1752-56.
- Konttinen, Y.T., Stegaev, V., Mackiewicz, Z., et al. (2010). Salivary glands — ‘an unisex organ’? Oral Dis, 16(7), 577-85.
- Pomari, E., Nardi, A., Fiore, C., et al. (2009). Transcriptional control of human organic anion transporting polypeptide 2B1 gene. J Steroid Biochem Mol Biol, 115(3-5), 146-52.
- Jezova, D., Hlavacova, N. (2008). Endocrine factors in stress and psychiatric disorders: Focus on anxiety and salivary steroids. Ann N Y Acad Sci, 1148, 495-503.
 Contact: Salimetrics (USA)
Contact: Salimetrics (USA)