Salimetrics High Sensitivity (HS) Assay #1-1802
The Salimetrics Salivary Estriol (17b-triol) ELISA kit was designed for the laboratory determination of estriol in saliva samples. By making use of Salimetrics reagents, this saliva assay kit is ideal for low-level saliva estriol detection/measures with exceptional sensitivity. All Salimetrics salivary immunoassay kits are manufactured by experts in assay design and proven to deliver better results for saliva biomarkers.Technical Summary
| Assay Protocol |
|---|
| Rev. 02.21.25
|
| Specifications | |
|---|---|
| Catalog#: | 1-1802 |
| Regulatory Status: | RUO |
| Format: | 96-well plate |
| Assay Time: | ~ 24 hrs |
| Sample Volume/Test: | 100 µL of X2 dilution |
| Sensitivity: | 1 pg/mL |
| Assay Range: | 5 pg/mL - 1215 pg/mL |
| Storage Requirements: | 2-8°C |
| Tests Per Kit | |
|---|---|
| Singlet: | 76 |
| Duplicate: | 38 |
| Target Analyte |
|---|
| Technical Documentation |
|---|
Salivary HS Estriol Assay Kit Overview
Intended Use
The Salimetrics Estriol/High Sensitivity (HS) Estriol Enzyme Immunoassay Kit is a competitive immunoassay specifically designed and validated for the quantitative measurement of salivary Estriol. It is not intended for diagnostic use. It is intended only for research use in humans and some animals. Salimetrics has not validated this kit for serum or plasma samples.
Introduction
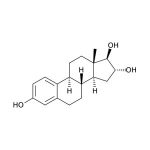
Estriol (1,3,5(10)-estratriene-3,16α,17β-triol; E3) is a female sex steroid hormone largely associated with pregnancy and fetal development. Fetal adrenal DHEA-S is metabolized in the fetal liver to 16-OH-DHEA-S, which is then converted to Estriol in the placenta. Near term, the fetus is the source of 90% of the 16-OH-DHEA-S in the normal human pregnancy. Maternal circulating Estriol levels rise progressively during pregnancy, reaching a peak in the third trimester. The physiological roles of Estriol in non-pregnant women are not well understood and are under investigation, particularly in connection with aging and post-menopausal health. With respect to estrogenic activity, Estriol is generally thought to be less potent than Estradiol or Estrone. However, with regard to nongenomic signaling pathways and functional responses in the pituitary, it has been pointed out that Estriol is a strong estrogen. In blood, the majority of Estriol is bound by serum proteins, with about 14-16% remaining unbound. Unbound Estriol enters saliva from blood via intracellular mechanisms, and correlation between serum and saliva samples is highly significant.
Salivary Estriol Assay Principle
This is a competitive immunoassay kit. Estriol in standards and samples compete with Estriol conjugated to horseradish peroxidase for the antibody binding sites on a microtitre plate. After incubation, unbound components are washed away. Bound Estriol Enzyme Conjugate is measured by the reaction of the horseradish peroxidase enzyme to the substrate tetramethylbenzidine (TMB). This reaction produces a blue color. A yellow color is formed after stopping the reaction with an acidic solution. The optical density is read on a standard plate reader at 450 nm. The amount of Estriol Enzyme Conjugate detected is inversely proportional to the amount of Estriol present in the sample.
References & Salivary Estriol Research
-
-
- Troisi, R., Potischman, N., Roberts, J.M., et al. (2003). Maternal serum oestrogen and androgen concentrations in preeclamptic and uncomplicated pregnancies. Int J Epidemiol, 32(3), 455-60.
- Reis, F.M., D’Antona, D., Petraglia, F. (2002). Predictive value of hormone measurements in maternal and fetal complications of pregnancy. Endocr Rev, 23(2), 230-57.
- Vining, R.F., McGinley, R., Rice, B.V. (1983). Saliva estriol measurements: An alternative to the assay of serum unconjugated estriol in assessing feto-placental function. J Clin Endocrinol Metab, 56(3), 454-60.
- Kirkish, L.S., Compton, A.A., McCann, D.S. (1986). Salivary estriol as an index to fetal wellbeing. Clin Chem, 32(1 Pt 1), 71-75.
- Heine, R.P., McGregor, J.A., Goodwin, T.M., et al. (2000). Serial salivary estriol to detect an increased risk of preterm birth. Obstet Gynecol, 96(4), 490-97.
- Weintrob, N., Drouin, J., Vallette-Kasic, S., et al. (2005). Low estriol levels in the maternal triple-marker screen as a predictor of isolated adrenocorticotropic hormone deficiency caused by a new mutation in the TPIT gene. Pediatrics, 117(2), e322-7.
- Canick, J.A., MacRae, A.R. (2005). Second trimester serum markers. Semin Perinatol, 29(4), 203-8.
- Watson, C.S., Jeng, Y.-J., Kochukov, M.Y. (2008). Nongenomic actions of estradiol compared with estrone and estriol in pituitary tumor cell signaling and proliferation. FASEB J, 22(9), 3328-36.
- Jacobson, H.I., Lemanski, N., Agarwal, A., et al. (2010). A proposed unified mechanism for the reduction of human breast cancer risk by the hormones of pregnancy. Cancer Prev Res (Phil Pa), 3(2), 212-20.
- Larfors, G., Lambert, P.C., Lambe, M., et al. (2009). Placental weight and breast cancer survival in young women. Cancer Epid Biomark Prev, 18(3), 777-83.
-
- Hickey, M., Saunders, C., Partridge, A., et al. (2008). Practical clinical guidelines for assessing and managing menopausal symptoms after breast cancer. Ann Oncol, 19(10), 1669-80.
- Mascarenhas, C., Lambe, M., Bellocco, R., et al. (2006). Use of hormone replacement therapy before and after ovarian cancer diagnosis and ovarian cancer survival. Int J Cancer, 119(12), 2907-15.
- MacMahon, B. (2006). Epidemiology and the causes of breast cancer. Int J Cancer, 118(10), 2373-78.
- Lagiou, P., Samoli, E., Lagiou, A., et al. (2005). Maternal height, pregnancy estriol and birth weight in reference to breast cancer risk in Boston and Shanghai. Int J Cancer, 117(3), 494-98.
- Kassi, E., Moutsatsou, P. (2010). Estrogen receptor signaling and its relationship to cytokines in systemic lupus erythematosus. J Biomed Biotech, 2010:317452.
- Ding, J., Zhu, B.T. (2007). Unique effect of the pregnancy hormone estriol on antigen-induced production of specific antibodies in female BALB/c mice. Steroids, 73(3), 289-98.
- Rovenský, J. (2006). Rheumatic diseases and Klinefelter’s syndrome: Review. Scripta Med (Brno), 79(4), 237-46.
- Sicotte, N.L., Liva, S.M., Klutch, R., et al. (2002). Treatment of multiple sclerosis with the pregnancy hormone estriol. Ann Neurol, 52(4), 421-28.
- Soldan, S.S., Alvarez-Retuerto, A.I., Sicotte, N.L., Voskuhl, R.R. (2003). Immune modulation in multiple sclerosis patients treated with the pregnancy hormone estriol. J Immunol, 171(11), 6267-74.
- Kika, G., Izumi, S.-I., Mori, A., et al. (2009). Beneficial aspect of oral estriol as hormone replacement therapy: Consideration on bone and lipid metabolism. Tokai J Exp Clin Med, 34(3), 92-98.
- Drača, S. (2006). Estriol and progesterone: A new role for sex hormones. Int J Biomed Sci, 2(4), 305-7.
- Moutsatsou, V., Oakey, R.E. (1988). Oestriol binding to plasma proteins. J Steroid Biochem, 29(3), 319-23.
- Vining, R.F., McGinley, R.A., Symons, R.G. (1983). Hormones in saliva: Mode of entry and consequent implications for clinical interpretation. Clin Chem, 29(10), 1752-56.
- Evans, J.J., Wilkinson, A.R., Aickin, D.R. (1984). Salivary estriol concentrations during normal pregnancies, and a comparison with plasma estriol. Clin Chem, 30(1), 120-21.
-
 Contact: Salimetrics (USA)
Contact: Salimetrics (USA)