Drop Date: April 2011
SBB – Salivary Biomarkers of Inflammation
In This Drop: Salivary Bioscience and Inflammation
 Bio-medical researchers routinely measure biomarkers such as cytokines (IL-6, IL-1ß, TNF-α) and C-reactive protein (CRP) in blood in order to assess the presence of inflammation. In order to avoid the cost, inconvenience, discomfort, and bio-hazard risk associated with blood drawing, however, researchers have more recently been exploring the utility of inflammatory markers in saliva.
Bio-medical researchers routinely measure biomarkers such as cytokines (IL-6, IL-1ß, TNF-α) and C-reactive protein (CRP) in blood in order to assess the presence of inflammation. In order to avoid the cost, inconvenience, discomfort, and bio-hazard risk associated with blood drawing, however, researchers have more recently been exploring the utility of inflammatory markers in saliva.
Studies involving salivary IL-6, IL-1ß, and TNF-α have been appearing with increasing frequency, and interesting associations to psychological and physiological stress have been observed, along with associations to local inflammatory conditions such as periodontitis, diseases of the salivary glands, and oral cancer. The relationships of salivary levels of these cytokines to blood levels are still not well understood, however, and initial studies have suggested there is only modest correlation between the two fluids.
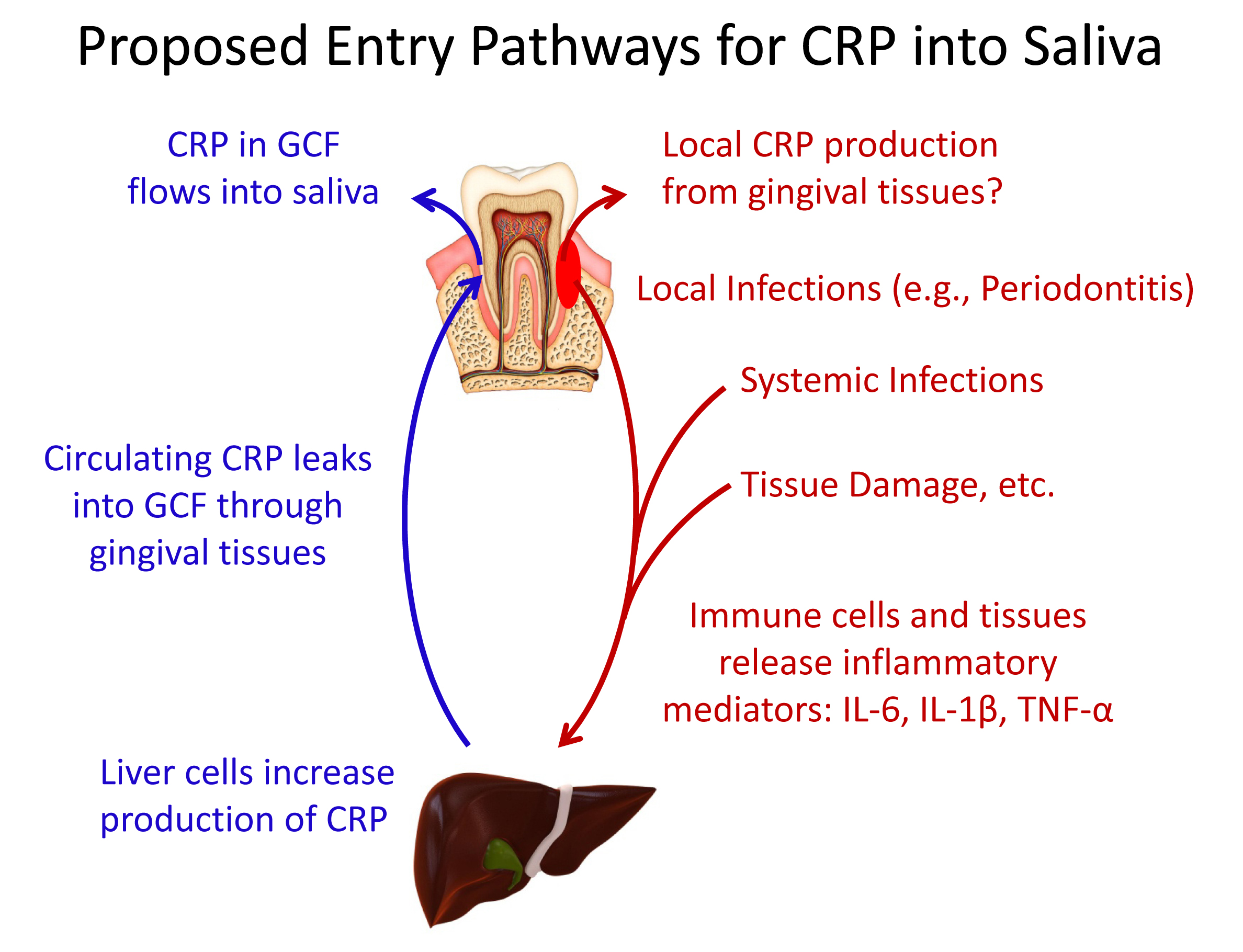
In the case of CRP, there is encouraging research that suggests salivary CRP may be more strongly associated with serum CRP than is true for other inflammatory markers. CRP, which originates largely from the liver, is too large a molecule to pass from the circulation into the salivary glands by diffusion or ultrafiltration as do many other salivary analytes, and it is believed that small amounts of CRP enter whole saliva mainly as a component of the gingival crevicular fluid (GCF) that flows out from the junctions between the teeth and gums. Whole saliva is much easier to collect than GCF, which could make saliva the oral fluid of choice for routine assessment of CRP in clinical or field studies.
As with the cytokines, however, the question of local production of CRP in the oral cavity must be considered, since it could potentially obscure the relationship between blood and salivary levels and the interpretation of salivary CRP in relation to other analytes of interest. In this issue of the Spit Report, we present several recent papers that examine the relationship between serum and salivary CRP, including a very recent study that is the first to report a moderately strong correlation between serum and salivary levels of CRP in humans.
Technical Advice
Collecting and Handling Saliva Samples for Cytokine Analysis
Advice on proper saliva collection methods and handling for salivary cytokines.
*Salimetrics provides this information for research use only (RUO). Information is not provided to promote off-label use of medical devices. Consult full text of article.
Featured Article
Validation of a High-Sensitivity Assay for C-Reactive Protein in Human Saliva.
Ouellet-Morin, I., Danese, A., Williams, B., & Arseneault, L. (2011). Brain Behav Immun, 25(4), 640-46.
With the recent introduction of a number of high-sensitivity immunoassays that can measure CRP in the range of values normally found in saliva, researchers have begun to evaluate salivary CRP for its utility as a non-invasive measure of systemic inflammation. This study is one of the first conducted with humans. Blood and unstimulated passive drool samples were collected from 61 healthy adult volunteers in order to investigate the correlation of salivary CRP with serum CRP. In addition, the study examined associations of salivary CRP with known correlates of systemic inflammation (serum IL-6, BMI, and smoking); stability of CRP in saliva was also studied.
Salivary CRP values – but not serum CRP values – for ten of the participants exceeded 2 standard deviations from the mean reported in healthy adults by the assay manufacturer. These high values were not found to be related to saliva flow rate, saliva pH, blood contamination, health conditions, or medications. It was determined that these high values were not caused by poor precision of the assay for samples with CRP values beyond the dynamic range of the assay. Consequently, the high CRP values for these individuals were not explainable, and they were excluded from the analysis. The authors speculate that local inflammatory processes in the mouth may have led to high values in these individuals. They suggest that future studies should therefore include a complete oral health examination as part of the participants’ health assessment.
As expected, the saliva-to-serum ratio was low (1:1633). This finding is consistent with belief that CRP has a restrictive pathway of entry into saliva mainly through gingival crevicular fluid. The correlation between serum and salivary CRP was found to be moderately strong, r = 0.72. The association did not vary by age or sex, but the prediction of serum CRP levels from salivary levels was more accurate at higher serum mean levels. Importantly, analysis of the data found that salivary CRP was able to predict accurately 89% of the participants with high serum CRP levels (cutoff > 3 mg/L), which is considered a good measure of discrimination. Salivary CRP was also found to be associated with elevated serum IL-6, high BMI, and smoking. Examination of the effect of different storage conditions found that salivary CRP is stable at room temperature for up to 8 hours. Freezing on the day of collection is advised, however, to avoid degradation that occurs under longer term storage.
In summary, this study provides important initial evidence suggesting that salivary CRP may provide a valid prediction of serum CRP. This finding of a moderately strong correlation between salivary and serum CRP in humans agrees with strong saliva-serum CRP correlations that have been reported recently in animal studies. Additional human studies are needed, however, in order to confirm the serum-saliva correlation found here in a broader range of populations with expected high or low CRP levels. The authors discuss, for example, another recent study involving human participants that found no correlation between serum and salivary CRP (Dillon, et al. 2010).
Research Area: Health & Inflammation
Focus: Inflammation & Immune Function
REFERENCES & RELATED RESEARCH
C-Reactive Protein in Gingival Crevicular Fluid may be Indicative of Systemic Inflammation.
Megson, E., Fitzsimmons, T., Charmapatni, K., & Bartold, P.M. (2010). J Clin Periodontol, 37(9), 787-804.
CRP was found in GCF and gingival tissue samples from periodontitis patients and from healthy controls. No gingival tissue samples had detectable amounts of CRP mRNA, however, suggesting that the CRP was of systemic origin. Levels of CRP varied considerably among individuals, and CRP was not found in all periodontitis sites; these findings agree with previous reports of non-uniformity in the systemic inflammatory response among individuals.
Research Area: Health & Inflammation
Focus: Inflammation & Immune Function
Human Gingiva is Another Site of C-Reactive Protein Formation.
Lu, Q., & Jin, L. (2010). J Clin Periodontol, 37(9), 789-96.
CRP was detected in gingival tissues from periodontitis patients and from healthy controls. CRP and IL-6 mRNAs were also detected in all gingival tissue samples; CRP gene expression was strongly correlated with IL-6 expression. A similar detection frequency of CRP in both healthy and periodontitis patients, significant variation of expression among individuals, and a highly interrelated expression pattern at diseased and healthy sites within individuals indicate that CRP expression is subject dependent. CRP mRNA and protein were detected in reconsituted human gingival epithelial cultures from three patients. The study shows that human gingival tissues are able to produce CRP, possibly in response to IL-6 activity in the tissues.
Research Area: Health & Inflammation
Focus: Inflammation & Immune Function
Use of Saliva-Based Nano-Biochip Tests for Acute Myocardial Infarction at the Point of Care: A Feasibility Study.
Floriano, P.N., Christodoulides, N., Miller, C.S., Ebersole, J.L., Spertus, J., Rose, B.G., Kinane, D.F., et al. (2009). Clin Chem, 55(8), 1530-38.
Biomarkers in unstimulated whole saliva were investigated for their potential to serve as markers of acute myocardial infarction (AMI). Both established and novel cardiac biomarkers demonstrated significant differences in concentrations between patients with AMI and controls without AMI. The saliva-based biomarker panel of C-reactive protein, myoglobin, and myeloperoxidase was found to have significant diagnostic capability. When combined with ECG, the panel yielded strong screening capacity for AMI.
Research Area: Health & Inflammation
Focus: Inflammation & Immune Function
*Note: Salimetrics provides this information for research use only (RUO). Information is not provided to promote off-label use of medical devices. Please consult the full-text article.
 Contact: Salimetrics (USA)
Contact: Salimetrics (USA)